http://www.ncbi.nlm.nih.gov/pubmed/25716226
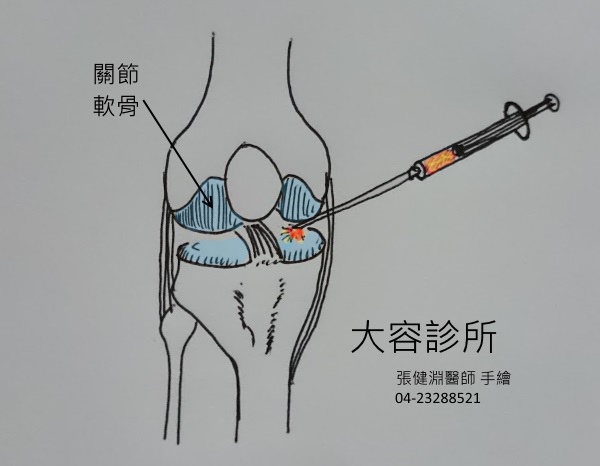
許多退化性關節炎的患者接受膝關節內的血小板注射治療(PRP)後, 獲得立即性的改善。這是為什麼呢?
如果由當初的原理來看, 膝關節內的血小板注射治療(PRP)目的在於利用血小板內富含的生長因子去刺激關節內受損的部份產生較多的修復機制(可參連結: PRP(高濃度血小板血漿)治療關節疾患 )。但是這種修復機制理論上不會在注射完後立即發生。
所以由本篇研究報告來看, 膝關節內的血小板注射治療(PRP)不單單只有刺激關節內的修復機制, 其實它也有抗發炎的作用, 讓退化性關節炎的發炎反應減少, 獲得較為立即的症狀改善效果。
依照這個理論的應用, 如果在發炎反應的部位, 如果不想使用抗發炎的藥物, 或者是不想使用太大量的抗發炎藥物, 使用血小板注射的方式也許也可以達到抗發炎的效果, 或是用做輔助其它抗發炎藥物。
此外, 於採血時, 無論是否包含白血球在內, 都是有相似的抗發炎反應, 並沒有因為白血球含量的多寡而有不同的結果。
原文大綱如下:
Platelet-Rich Plasma Increases Anti-inflammatory Markers in a Human Coculture Model for Osteoarthritis.
Abstract
BACKGROUND:
Platelet-rich plasma (PRP) has anti-inflammatory effects with potential applications in the treatment of osteoarthritis (OA).
PURPOSE:
To use an in vitro coculture model of OA in human cartilage and synovium to investigate the anti-inflammatory effects of 2 different PRP preparations.
STUDY DESIGN:
Controlled laboratory study.
METHODS:
A coculture system was created using osteoarthritic cartilage and synovium from 9 patients undergoing total knee arthroplasty. Interleukin-1β (IL-1β) was added to each coculture to induce inflammation. Two PRP preparations were obtained-one yielding low white blood cell and platelet concentrations (PRPLP) and one yielding high platelet and white blood cell concentrations (PRPHP). Either PRPLP, PRPHP, or medium was added to the coculture wells. Control wells contained OA cartilage and synovium but neither IL-1β nor PRP. Normal, non-OA cartilage was obtained to establish baseline gene expression levels. Quantitative polymerase chain reaction was used to measure changes in markers of inflammation in the tissues (a disintegrin and metalloproteinase with thrombospondin motifs-5 [ADAMTS-5], tissue inhibitor of metalloproteinases-1 [TIMP-1], vascular endothelial growth factor [VEGF], aggrecan, and type I collagen) at 0, 24, 48, and 72 hours.
RESULTS:
Treatment with PRPLP or PRPHP significantly decreased expression of TIMP-1 and ADAMTS-5 in cartilage, increased aggrecan expression in cartilage, and decreased ADAMTS-5, VEGF, and TIMP-1 expression in synovium compared with control cocultures (P < .05). There was significantly less nitric oxide production in the PRPLP and PRPHP groups compared with controls (P < .05). There were significant differences in gene expression in the normal cartilage compared with all 4 groups of OA cartilage at all 4 time points. Treatment with either PRPLP or PRPHP returned some gene expression to the same levels in normal cartilage but not for all markers of inflammation.
CONCLUSION:
This coculture model assessed 2 different PRP preparations and their anti-inflammatory effects over time on human OA cartilage and synovium. Both had a significant anti-inflammatory effect on gene expression; however, there was no difference in the anti-inflammatory effect between the 2 preparations.
CLINICAL RELEVANCE:
Osteoarthritis is a leading cause of chronic disability, and less invasive treatment methods are needed. Study results suggest that PRP injections may be an effective alternative anti-inflammatory agent in the treatment of OA.
© 2015 The Author(s).
KEYWORDS:
osteoarthritis; platelet-rich plasma
- PMID:
- 25716226
- [PubMed - as supplied by publisher]




 留言列表
留言列表
